Standard Care – a key to improving medical outcomes
Through efforts great and small, healthcare providers are advancing patient safety

Just a few years ago, days after Thanksgiving, a woman was retaining fluid from dialysis and went to a hospital in Houston for emergency assistance. The woman required a blood transfusion which was subsequently ordered by hospital staff. A disaster was averted when the hospital’s lab caught an error in the request. The staff who had placed the order had inadvertently included another patient’s blood type. If the lab staff hadn’t caught the error, the mistake could have seriously injured the patient.1
Unfortunately, a few days later, a similar mistake was made with a different patient. This time, the lab didn’t catch the error and a woman was given the blood transfusion meant for another patient. The woman given the wrong blood type died the next day from cardiac arrest.
That incident, and others that followed a similar pattern at the hospital, led to negative consequences from the government, the media and the public. The hospital responded by putting several new programs in place to prevent similar events from happening again.
This is only one of many similar incidents that have taken place in hospitals across the country. Despite the best intentions of practitioners, medical errors may account for as few as 44,0002 to as many as 250,0003 deaths per year in the US. If the latter is true, and there is some debate on the matter,2 medical errors may be the third leading cause of death in the US.
When the care of a single individual is spread across multiple teams of doctors, nurses, specialists and other employees who make hospitals function, it’s easy to understand how mistakes can be made. In response, professionals working within healthcare are investing a tremendous amount of resources to improve patient safety and quality of care.
Those efforts appear to be paying off. The U.S. Department of Health & Human Services’ Agency for Healthcare Research and Quality (AHRQ) published4 this infographic indicating a decline in hospital acquired conditions.
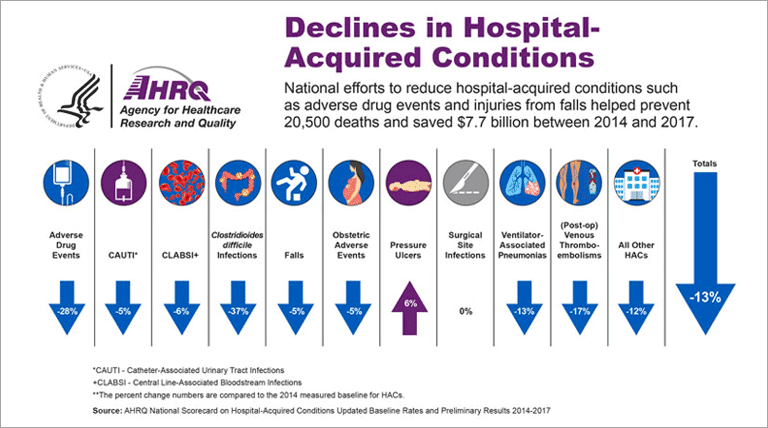
Initiatives that are making a difference
Through efforts great and small, government organizations, professional groups, health systems and individual care providers are confronting the issue of patient safety and quality of care head on. Many of these efforts focus on a common standard that, when applied accurately, have greatly diminished the number of adverse events.
MedStar Health, a large health system serving the Baltimore-Washington metro region has taken a particularly proactive stance on patient safety. Through a combination of several techniques to reduce risk and preventable harm, MedStar was able to lower their number of serious safety events by almost 60% from 2012-2016.5
One of the most effective programs applied by MedStar is the Communication and Optimal Resolution (CANDOR) process. The detailed process helps providers “respond in a timely, thorough, and just way when unexpected events cause patient harm.”6
MedStar has invested heavily in developing expertise in quality and safety and is actively sharing their learnings with other health systems around the world through the MedStar Institute for Quality and Safety.
Not all initiatives to improve patient care need be as ambitious as those being pursued at MedStar.
Since 2010, Seattle Children’s Hospital has been continuously deploying clinical standard work pathways to reduce variation in care and improve patient safety.7
Every patient is different, but diseases aren’t always. Following these evidence-based practices means patients consistently receive the safest and most effective care.
For patients with a predictable clinical course, the pathways help guide care providers in treatment. The standard processes have helped providers quickly see what is effective and what is not in treating patients, freeing them to be more creative when needed.
Within five years, the hospital had 39 pathways in place. Today, that number has nearly doubled with more than 70 pathways in use throughout the hospital.8
Even far simpler programs have shown promising results in improving patient outcomes. Consider the power of the humble checklist.
While likely not the first person to consider using checklists in clinical work, Peter Pronovost, MD, PhD is arguably the first to popularize the checklist as a simple tool that can bring about significant results.
In a 2006 study9, Pronovost and his team showed that following 5 simple steps would prevent catheter-related bloodstream infections. In fact, “[g]iven the results of the study, many of the estimated 80,000 infections, up to 28,000 deaths, and $2.3 billion in costs attributed to these infections annually in the United States could be reduced” without implementing new technology or adding staff.
In 2009 Atul Gawande, MD, MPH published his New York Times bestselling book The Checklist Manifesto.10 The book recounts many different scenarios (including the one above) where checklists have been used to simplify processes and avoid errors.
Gawande’s own experience introducing checklists into surgical workflow at hospitals in multiple countries of different socioeconomic levels indicated a reduction in morbidity and mortality.11
Additional research seems to reinforce the idea that checklist usage during surgery12, after surgery13 and in many other clinical scenarios can have significant positive impact on patient outcomes.
Challenges yet to overcome
The common thread tying the success of all these initiatives together seems to be consistency of application and sustainability of the practice over time. Identifying best practices is helpful, but practicing them across teams, hospitals and systems over months and years can be more challenging.
Acadia provides a platform on which to build clinical procedures – from simple daily routines performed by one care provider, to more complicated clinical pathways used by teams.
For example, below is a diagram from a clinical pathway for assessment and treatment of pediatric viral bronchiolitis from Children’s Hospital of Colorado14:
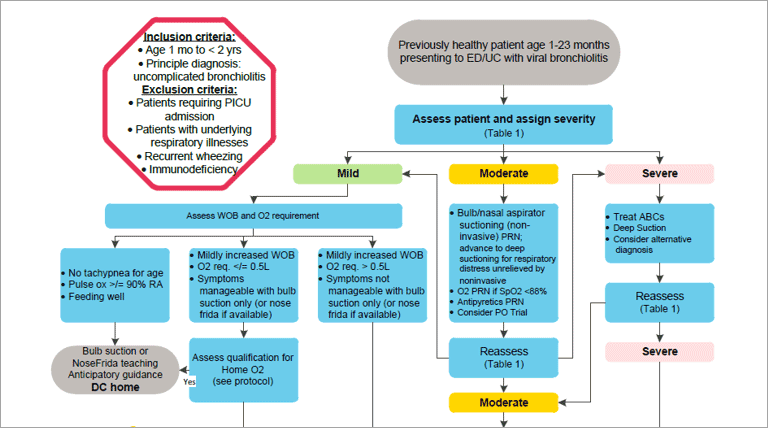
The hospital uses these clinical pathways to assist clinicians in standardizing the evaluation, diagnosis, and care of patients with specific conditions.15 Imagine taking these best practices beyond reference and inserting them directly into daily workflow.
Using Acadia, hospitals can assign each step of a pathway to individuals or teams of doctors, nurses and other specialists. Each process outlined in the workflow above could be converted into a task list that includes warnings, reference material, coding references and other important information. As each step of the process is completed, assignments can be passed to the next person or team in the workflow based on the decision reached by the previous provider(s).
This content can be searched from mobile medical carts, tablets or phones, making it easy for the right provider to find the information they need at the moment they need it.
The system is fully auditable to ensure that each step is accounted for and there is no gap in coverage. Providers also have the ability to identify opportunities to improve procedures and funnel that feedback to managers – allowing each pathway to be improved over time.
With a system in place to help manage the standard work, providers can be freed to use creativity when addressing individual patient needs that fall outside of the standard.
Sources:
- Numerous Mistakes Led to Fatal Blood Transfusion at St. Luke’s in Houston, Report Finds
- Medical error – the third leading cause of death in the US.
- Study Suggests Medical Errors Now Third Leading Cause of Death in the U.S.
- Declines in Hospital-Acquired Conditions
- Best Practices: Addressing errors with Candor
- Communication and Optimal Resolution (CANDOR) Toolkit
- Standardized Clinical Pathways for Hospitalized Children and Outcomes
- Clinical Standard Work Pathways and Tools
- An Intervention to Decrease Catheter-Related Bloodstream Infections in the ICU
- The Checklist Manifesto: How to Get Things Right
- A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population
- Strategies for Improving Surgical Quality — Checklists and Beyond
- Effect of a Comprehensive Surgical Safety System on Patient Outcomes
- Bronchiolitis | Inpatient
- What are Clinical Pathways?
Ready to crush your goals?
"*" indicates required fields